What Are Some of the Signs and Symptoms of Ph+ CML?
Some people may experience 1 or more of these symptoms before being diagnosed with Ph+ CML:
These are not all the symptoms of Ph+ CML. You may experience others. Call your doctor or HCP if you have any of the symptoms above or have any questions or concerns.
Most people are diagnosed in the earliest phase, known as the chronic phase (CP). Symptoms are milder or not noticeable in the CP compared with later phases.
What Are the CML Phases?
CML has 3 phases:
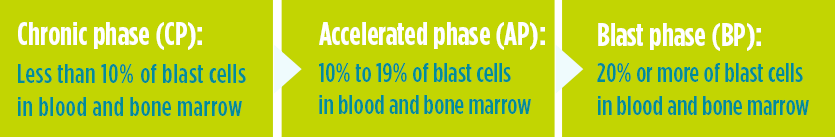
The phase definitions above are from the World Health Organization (WHO). Some doctors or HCPs may use different definitions. Talk to your doctor or HCP about any questions or concerns you may have about the different phases.
Most patients are diagnosed in the CP, so the goal of treatment is to control the disease in CP and keep it from getting worse for as long as possible. By blocking BCR-ABL, medicines called tyrosine kinase inhibitors (TKIs), like BOSULIF® (bosutinib), help slow the growth of CML cells.
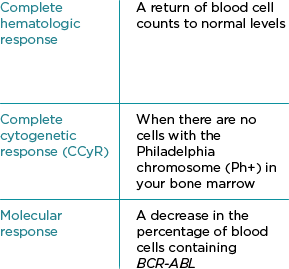
Monitoring During Therapy
Frequent monitoring and blood tests are very important, so ask your doctor about getting tests that gauge the status of your disease and how you are responding to treatment. Monitoring with quantitative polymerase chain reaction (qPCR) every 3 months is recommended for all patients after initiating therapy, including those who meet response milestones at 3, 6, and 12 months.
In CML, qPCR measures the number of cells that have the BCR-ABL cancer gene.*
qPCR-International Scale (IS) is how many BCR-ABL cells you have in your blood compared to baseline. After BCR-ABL >0.1%-1% has been achieved, molecular monitoring is recommended every 3 months for 2 years and every 3 to 6 months thereafter.*
*Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Chronic Myeloid Leukemia V.1.2024. © National Comprehensive Cancer Network, Inc. 2023. All rights reserved. Accessed October 30, 2023. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
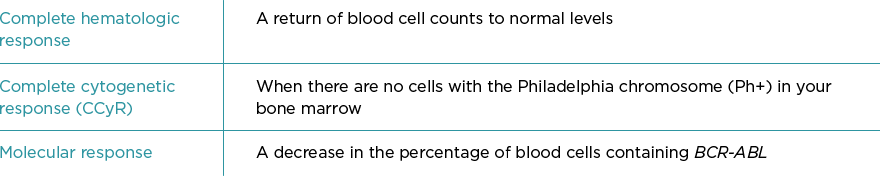
Two types of responses your doctor may mention are EMR and MMR
- EMR is early molecular response, which means that at
3 and 6 months, the amount of BCR-ABL in your
blood is ≤10% of when you started treatment - MMR is major molecular response, which means the
amount of BCR-ABL is ≤0.1% of what it was
at baseline
Your doctor may also order blood tests:
- To monitor your blood cell counts regularly during your treatment with BOSULIF. Call your doctor right
away if you have unexpected bleeding or bruising, blood in your urine or stools, fever, or any signs of
an infection - To monitor your liver function regularly during your treatment with BOSULIF. Call your doctor right away if
your skin or the white part of your eyes turns yellow (jaundice) or you have dark “tea color” urine
If you have multiple medical conditions, it is very important to have regular checkups to monitor these medical
conditions and your overall health. These medical conditions may include:
- Heart disease
- Kidney disease
- Lung disease
- Pregnancy
- High blood pressure
- Diabetes
Remember, the more information your doctor or HCP has, the better he or she will be able to make decisions
about what the best course of treatment is to manage your CML.

Resistance and Intolerance
What is resistance?
Resistance is when the disease fails to respond or stops responding to a given therapy. Your
doctor or HCP will schedule regular check-ups to measure your response to therapy. This will
be done using blood and bone marrow tests.
Resistance can occur at any time during treatment, even if you have been taking your
medicine successfully for several years. Because of this, resistance may be a possible cause
for not meeting treatment goals.
What is intolerance?
Intolerance is when a patient can no longer take his or her current medicine due to side
effects. If your side effects are severe, occur too often, or are damaging to your health, your
doctor or HCP may switch you to another medicine.
However, having side effects does not always mean that treatment should be switched. Often,
your doctor or HCP will be able to treat or manage side effects (for example, by reducing your
dose) without having to switch your medicine for Ph+ CML. Always tell your doctor or HCP if
you have side effects, even if you think they aren’t serious.